Digestion
Gut Health Library
The Gut Health Libraries [GHL'] © are protected by Copyright law. You do not have permission to print, copy, share, screenshot, reproduce, distribute or disseminate all, or any part, of the visual or written information. While due care has been taken to ensure the accuracy of the information contained herein, the information is made available on the understanding that Natalie Woodman is not providing professional advice on any particular matter or indicating a particular course of action. Nothing contained herein is intended to be used as medical or health advice and it is not intended to be used to diagnose, treat, cure or prevent any condition, nor should it be used for therapeutic purposes or as a substitute for your own health professional(s) advice. Before relying on any information, users should seek professional advice relevant to their particular circumstances. In some cases, the information may incorporate or summarise views, guidelines or recommendations of third parties. Such information is assembled in good faith but does not necessarily reflect the considered views of Natalie Woodman.
Click on the TOPIC below and it will take you to that section…
I have bloating and/or flatulence (gas). What causes it? How Can I relieve it?
What causes it… Abdominal bloating (along with concurrent 'gas') and (sometimes) accompanying pain has many possible causes such as hormonal, functional bowel disorders (IBS & IBD), Over-exercise, Dehydration, Increased Fibre intake, Cruciferous vegetables (e.g. Broccoli, Cabbage, Cauliflower), Shift Work, Sleep debt or interruptions, Malabsorption issues, Fluid retention (from salt), Overeating, Constipation (Fear - holding on), Eating too fast, Talking while eating, Carbonated drinks (soda & sparkling water), Gastrointestinal infection, Pregnancy, Medications and Dysbiosis (imbalance in the Gut Microbiome).
However, it has been concluded that one of the MAIN contributors to BLOATING is stress. Stress contributes to the initiation of altered gut motility and results in symptoms such as distension of the abdomen ‘bloating’, smooth muscle spasm, pain and bowel irregularities. Symptoms may not start until days or weeks after the ‘event’ and symptoms may persist long after the inflammation has resolved.
This leads to altered gut motility and the way food is broken down (i.e. how much time it spends in the stomach or the small intestines) and this can result in gas building up in the stomach, small and large intestines.
Sometimes if there is too much gas it can build up and be forced back up into the stomach i.e. heartburn/reflux/burping.
It can make the mid-lower abdominal region swell, look misshapen, be hard to touch, result in muscle spasm and can result in alot of flatulence (sometimes smelly, sometimes just non-odourous gas).
It can be MILD and TRANSIENT and cycle in and out during your program as your Gut Microbiome moves from a state of 'dysbiosis' (imbalance) to eubiosis (balance) and as it becomes accustomed to the increased amount of fibre (probably A LOT more than you've EVER eaten) It is an important factor to take into account in the first few weeks where you can feel like the 'bloating' and 'gas' are relentless.
Note: if bloating is accompanied by sharp pains, chronic diarrhoea or constipation, fever and/or blood in stools then you should seek medical advice as it could indicate a serious infection.
How to relieve it… Here are some of the factors that may be involved and some tips to help relieve. While ALL these factors should be paid attention to, the first THREE are generally the most common reasons for bloating...
Eating too fast, or eating while doing other things e.g. watching TV, scrolling on your phone etc. doesn't allow the digestive (gastric) juices to come out in time to break down food. In Module 2 we will be take you through Digestive Dominoes and discuss the importance of how and where you eat. But in the meantime, ensure that you are sitting down to eat, in a calm environment (perform deep breathing first) and then look and smell your food, chew slowly, and put your cutlery down between mouthfuls. AND do NOTHING while eating i.e. don’t scroll your phone, or stuff in mouthfuls between emails or computer work!! This IS an essential part of digestion and needed to minimize bloating due to the high intake of fibre.
Stress which doesn't necessarily mean a life changing event. But the non-obvious stressors like overthinking, overwhelm, fear, resentment, anger, worry, nervousness, the to do lists in your head etc. Stress is well known to affect digestive secretions and the production of enzymes that break down food. It also affects gut motility and is linked to both diarrhoea and constipation, bloating and gas. Stress can also alter sleep patterns and the circadian rhythm of the body due to sleep debt caused by disrupted sleep which in turn negatively affects the circadian rhythm of digestion!
Over-exercise can cause undue stress on the body especially when it is stressed internally from your health condition. So focus on your Barefoot walking, Yin Yoga and Resonant breathing.
Dehydration. You need to stay 'regularly' hydrated. 9-litres of water is needed to assist in digestion (you don’t need to drink 9-litres) that’s just what the body utilizes for the process. So follow your stretch-decompress-hydrate method to ensure regular hydration.
Talking too much while eating. Avoid talking while eating as it can increase the amount of 'gas' due to the fact that you swallow air while talking.
Eating too much. Try eating smaller meals, more frequently. Example: Halve your lunch and have half at lunchtime and the other half 2-3 hrs later. Halve dinner, then eat the other half an hour or so later, rather than a snack.
Chewing Gum? Easy fixed, don't chew gum (which you shouldn't be doing as it is an AVOID food while on your program). Chewing gum turns on the 'digestive juices' tap but there is nothing to break down except sugar components. This causes damage to the stomach and has a negative effect on your gut eco system, digestive enzymes and gastrointestinal integrity.
Drinking through a straw. This causes you to swallow to much air. Easy fixed, don't use a straw to drink.
Carbonated drinks. Avoid carbonated drinks such as soda, mineral or sparking water as they increase 'gas' in the stomach.
Cold or Hot drink consumption. Drinking COLD drinks or HOT drinks have an effect on gastric emptying and thus may alter the required time for gastric juices to break down food. Stay away from COLD drinks e.g. drink room temperature water AND stay away from HOT drinks and instead drink WARM herbal teas. WARM equals body temperature of around 37°C (98.6°F).
Targeted intervention while working on factors above…
Organic Ginger Root tea is always your first line of treatment as it helps to address gastrointestinal motility without affecting gastric emptying. It can assist with relieving indigestion, poor appetite and spasms of the gastrointestinal tract. Sip on throughout the day.
Herbal teas that can assist with bloating, and associated discomfort of gas, are Organic Chamomile, Fennel, Lemon balm, Peppermint* leaves or Organic Relaxation blend tea (remember to use GHC10 to get your 10% discount) NOTE: This is not a cure but rather to provide 'some' relief while you are improving your gut health. *Peppermint should be omitted if you suffer from heartburn, indigestion or reflux as it relaxes the lower esophageal sphincter.
Move every 30-minutes as regular movement is essential for gut motility. Sitting in the same position for a prolonged time can compress the digestive organs and result in sluggish digestion and subsequent bloating. Are you sitting at your computer? On the sofa for extended periods on your phone or watching TV?
Sit upright while working at your desk. Slowly twist your body, moving your shoulders and body (while hips and bottom remain stable) to the right, hold and then repeat on the left. Do 10-15 times.
Sit on the floor with both legs straight out in front of you, take your left leg bend at the knee and cross it over your right leg keeping your left foot on the floor right next to your right knee. Turn in the opposite direction, stretch and hold. Repeat on the other side. Do 10-15 times.
Sit upright, put your left hand on your hip and raise the right arm straight above your head. Then with the stretched right arm gently reach left so that you feel a stretch on the right side of your body. Breath in and out while out while you hold the stretch. Repeat 5-10 times on each side.
Have a warm bath and relax. Add some Epsom salts if you wish.
Avoid taking digestive enzymes or bitters (either pill or tonic form). You can try having a small salad* with 'bitter greens' that naturally support the release of gastric juices - prior to eating your meal. As bitter greens are ALSO prebiotics they further stimulate the growth of beneficial gut bacteria - something that supplements and tonics do NOT do! Examples of excellent bitter greens are... Rocket/Arugula, Alfalfa sprouts, Broccoli sprouts, Dill, Dandelion leaves, Radicchio/Chicory, Mint leaves and Endive. Make a small salad to eat prior to your meal with a mix of greens and a dressing made with squeezed lemon or lime over the top.
Avoid drinking coffee, instead try Dandelion root organic tea a bitter tea which supports digestive secretions, motility and detoxification. Studies show that the pungent compounds of dandelion also beneficially enhance mucosal protection. Collectively these two compounds are known to improve the microbial terrain.
NOTE: Shift workers have a greater susceptibility to gastrointestinal problems (e.g., irritable bowel syndrome incl. bloating, abdominal pains, alternating bowel movements). The higher rate of 'gut' issues is common among night workers and is partly due to a reduced gastrointestinal response after meals taken at night e.g. the absorptive capacity is less 'willing' to handle food consumed at night. Avoid eating, or at least restrict energy intake, between midnight and 06.00 hours, and try to eat at the beginning and end of the shift. Avoid a 'large meal' after your shift (breakfast) and before sleeping.
I have Heartburn/Reflux. What causes it? And How Can I relieve it?
First it’s important to understand the various ‘parts’ involved…. Just above the entrance to the stomach, lies a ring of tissue, a muscle called the Lower Esophageal Sphincter (LES). The LES is controlled by nerves within the oesophagus that relay information between the stomach and the brain.
When functioning properly Heartburn and reflux are non-existent. When not functioning properly it becomes the main player in heartburn and reflux, giving you a burning chest pain, and in some instances nauseousness when food makes its way back up the esophagus to the mouth.
In modern day life, the incidence of Heartburn has increased exponentially leading to a billion-dollar industry in antacid medication. However, this just makes the problem worse as antacids (PPI’s and over-the-counter liquid or lozenge medications) alter the pH of the stomach and proximal Duodenum affecting the pH dependent enzymes and gastric juices and the absorption and assimilation of Protein, Vitamin B12, Iron, Magnesium and Calcium. In the stomach, a single oral PPI dose will raise gastric pH, in most individuals, from 2.0 to over 6.0, a 10,000-fold change.
PPIs and antacids, also have the potential to influence the microbiome through pH-independent mechanisms….
First, proton pump inhibitors induce hormonal changes alter the gastrointestinal bacterial milieu.
Second, PPIs can alter lumenal contents to interfere with nutrient absorption and change the amount or location of bacterial food substrates.
Finally, PPIs contribute to elevate the activity of the pathogenic bacterium, H. pylori.
So, why are you possibly getting heartburn, or reflux, and what can you do?
Well you now understand the body ‘part’ involved (LES) but now need to understand what is happening physiologically within the body, when eating and digesting food.
When you take a mouthful of food, chew and swallow, peristaltic waves move the food along the esophagus and the LES relaxes to allow food to enter the stomach.
Once food enters the stomach, and the acidity of the stomach increases (going from a pH of 5-6.5) to a highly acidic pH of approx. 1.5−2.5 even down to 1.0pH.. messages from the stomach go back to the brain and constrict the LES, basically creating a seal so that the stomach's contents stay in the stomach and nothing in the stomach (like stomach acid) splashes up and into the esophagus causing heartburn and/or reflux.
However, when the LES remains partially open, or re-opens, and acid splashes up — it can cause a burning sensation and pain.
The causative factors are...
Build-up of stomach gas... can happen when eating quickly, drinking carbonated/cold drinks or while eating and/or talking a lot whilst eating. Forces air up through the stomach and into the esophagus, relaxing the LES.
Vagus nerve dysfunction… is a common factor in reflux symptoms. Vagal nerve dysfunction can arise out of a previous infection, previous or current inflammation, physical or psychological (mental) stress. The vagus nerve plays a central role in the bidirectional transmission and mediation of sensory information between the brain and the body. The signalling of systemic inflammation is communicated to the brain via neural (predominantly vagus nerve) pathways.
Pregnancy… due to pressure of the growing foetus against the stomach and also hormones circulating through the body.
Overeating… when overeating (often due to eating too fast) the stomach swells and places extra pressure on the LES.
Being overweight… places extra pressure on the area and causes the LES to lose strength.
Caffeine/Tannins… affect stomach acidity and thus the LES.
Alcohol… relaxes the LES and over time reduces its ability to close. Over time this can result in considerable damage.
Medications… such as, Antidepressants, Iron supplements, Blood pressure medications, Sleeping pills and long-term use of Antacids/Proton pump inhibitors (PPIs). Research shows that long-term use of Antacids can not only reduce the diversity of bacterial communities in the gut through alteration of the pH of your intestinal lumin (lining) but is a risk factor in developing Gastrointestinal disorders, infections and vitamin and mineral deficiencies.
Hormone Replacement Therapy (HRT)… puts you at much higher risk of developing Gastroesophageal reflux disease (GERD).
Antibiotics… through widespread antibiotic use, the complex microbial community in the distal oesophagus has been altered and led to a predominance in gram-negative (pathogenic) bacteria.
Fatty and Oily foods... cause the LES to relax.
Indirectly though infections... such as H.Pylori, which can disrupt stomach acid production.
Stress... (worry, anxiety, overthinking, overwhelm, anger, fear etc.) alters the brain-gut axis (BGA) and thus alters stomach gastric secretions. In fact, "A consequence of the dysregulation of BGA induced by exposure to stress may lead to the development of a broad array of gastrointestinal diseases such as gastroesophageal reflux disease (GERD), peptic ulcer disease (PUD), IBD, IBS and even food allergy."
Smoking... either cigarettes or marijuana, can damage the LES membranes causing it to weaken. It also affects stomach acidity.
What to do to reduce and eliminate Heartburn and Reflux..
✅ Practice Digestive Dominoes EVERY time you eat. From Looking and smelling at your food through to putting cutlery down, being calm (perform deep breathing first) and doing NOTHING while eating. This IS an essential part of digestion and proper functioning of the LES. Without doing this, it is not going to improve!
⚠️ Reduce stress ESPECIALLY around eating times. Practice your resonant breathing before, during and after eating. "Gastroesophageal reflux disease (GERD) represents one of the most important manifestations of stress exposure to GI tract... the reduction of stress may lead to an improvement of GERD symptoms”
🚫 Avoid drinking carbonated drinks such as Soda or Sparkling Water, before, during or after dinner, as it increases gas in the stomach.
🚫 Avoid drinking Peppermint Tea as it can relax the LES.
🚫 Avoid drinking anything with Caffeine in it (coffee/tea) within a couple of hours of eating as it may relax the LES.
🚫 Eliminate citrus foods (for a while) and see if it helps. In some individuals this can cause issues with the LES. Swap morning Lemon Blend to Organic Ginger Root tea.
✅ Drink Organic Ginger root tea slowly and regularly as it can assist with stomach acidity and may assist in tightening the LES.
✅ Practice Resonant breathing for at least 5-minutes. Studies confirm positive effects of slow deep abdominal breathing on gastroesophageal reflux disease. Research shows that individuals… “who breathe at half their normal rate are able to decrease pain and depressive symptoms more than when they are breathing normally” … and… “cardio-respiratory stimulation of the vagus nerve may explain some of the overall positive emotional and cognitive benefits”
✅ Go for a barefoot walk, do your resonant breathing and (if you can make the time) 5-10 minute Yin Yoga movements.
✅ Replace caffeinated drinks with Ginger, Chamomile, Liquorice or Fennel tea.
✅ Ensure you sit upright (not hunched over) when eating, and stay upright (not slunk on the sofa) for at least 1-2hrs after eating. Don't lay down flat. If you need to go to bed, then elevate the mattress by placing pillows under it.
⚠️If after doing ALL of this continually for a few weeks, this the condition persists, then further medical investigation is warranted for H.Pylori, Parasites and or a functional disorder.
Can you please explain the liver detoxification process?
The liver’s primary job (it does other stuff too) is to detoxify toxic substances such as components of food chemicals (like those found in non-organic and processed foods), chemical based personal care and home-care products, over the counter and prescribed medications, and environmental toxins such as exhaust fumes, hazardous herbicides, pesticides, chemicals etc.
The liver processes these AND eliminates them through urine, faeces and sweat.
The liver performs this role around the clock (24/7), so thinking you are ‘detoxing’ right now because of a headache etc. is actually a myth, your liver is ALWAYS detoxifying harmful substances and clearing them. If it didn’t… toxins would build up and you’d be in need of serious medical intervention!
You CANNOT detox yourself, nor speed up the process, but you CAN support your body (especially your liver) with ALL it needs so that toxins can be eliminated safely and without you experiencing adverse reactions or symptoms.
The liver detoxifies substances from a ‘toxic’ substance (e.g. something that will harm your body and organs) to a ‘safe’ substance so it can be excreted. It does this in a TWO phase process...
PHASE ONE: Liver cells contain Cytochrome P450 enzymes that perform many jobs, but one of the jobs it ‘specializes’ in is taking ‘toxins’ and breaking them down so they can be excreted through Oxidation → Reduction → Hydrolysis → Hydration → Dehalogenation. In a nutshell --- it takes fat soluble toxins and changes them to water-soluble waste products so it can be excreted through the kidneys, bowels and sometimes sweat.
In this phase, these ‘toxins’ are only partially transformed and can be potentially more harmful than the original toxins. They can be very reactive and can cause secondary tissue damage, especially inflammation.
So, it is ESSENTIAL that the LIVER has a wide variety of nutrients to protect itself from these ‘toxins’ and also provide it with what it needs to do its job properly.
NUTRIENTS required – Protein (Amino acids e.g. Cysteine), Vitamins A (caretoids), Vitamins B, C, D3, E. Minerals such as Zinc, Selenium, Molybdenum, Calcium, Copper, Manganese, Magnesium. Thiols, Bioflavonoids, Folic acid, Glutathione, Antioxidants. Not to mention all important FIBRE because…
“The liver is a central immunological organ that is particularly enriched in innate immune cells and constantly exposed to circulating nutrients and endotoxins derived from the gut microbiota”
“The delicate interaction between the gut and liver prevents accidental immune activation against otherwise harmless antigens”
“The intestinal microbiota and bacterial products may contribute to the development of liver diseases through multiple mechanisms including increased intestinal permeability, chronics ystemic inflammation, production of short-chain fatty acids and changes in metabolism.”
So, where do you get all these nutrients from? You guessed it PLANTS! Whole foods such as fruits, vegetables, nuts, seeds, beans, legumes and whole grains.
But I know you're thinking..."BUT which one do I need more of?" OR "how about I take a detox supplement ?"
Answer... you don't need more of ANY one nutrient, you need them all. And ALL of them are naturally occurring in whole plant based foods!!
Once the liver has successfully completed Phase 1, it moves to…
PHASE TWO: A series of reactions whereby highly reactive ‘toxic’ water-soluble metabolites are turned into non-toxic products for elimination by the kidneys (urine), gall bladder – bile - bowels (faeces), skin (sweat).
To be able to perform the necessary functions of….Sulfation → Glucuronidation → Glutathione Conjugation → Acetylation → Methylation → Amino acid Conjugation… yep you guessed it, the liver needs nutrients.
Examples…. Sulphur containing foods such as onions, garlic, cruciferous vegetables. Limonene containing foods such as citrus peel, peppermint, dill, caraway, fennel and celery. Vitamin B containing foods (nearly all vegetables and grains), Selenium (Brazil nuts but in heaps of foods), Zinc (nuts and seeds), Folic acid (Cruciferous veggies, especially cabbage), and precursors of glutathione which are the sulphur containing amino acids N-acetyl cysteine and methionine – all available from a WIDE range of whole plant-based foods.
Get it?
Maybe someone has suggested a ‘Detox kit’ or a 'Supplement'? They tell you it will 'support the liver', 'cleanse the liver/body' or 'help with quick detox'???
I am telling you categorically that it CANNOT provide the body with the entire spectrum of nutrients required for safe, and effective, liver detoxification. What it DOES do is empty your wallet of your hard earned dollars! Spend $40 on a useless supplement or $40 on a basket full of useful and effective fresh whole plant-based foods!!
IF you REALLY want to support your liver then....
Keep eating all the food on your program. It is rich in ALL these NUTRIENTS that are NEEDED to support the liver PLUS ALL IMPORTANT soluble and insoluble fibre that works to keep ‘elimination’ smooth and regular which is essential for the body to rid itself of toxins.
Do your stretch-decompress-hydrate method each day to ensure you are getting a regular small amount of hydration.
Swap one of your coffee’s, or black tea, to a herbal teas such as Fennel, Ginger, Peppermint, Chicory or Dandelion root tea to support the kidneys, bowels and skin as they eliminate these toxins.
Do not drink ALCOHOL which all place a stress on the liver, introduces a high amount of toxins, and harms it’s ability to function.
Practice resonant breathing as soon as you become aware of a stress. Reason being is that ‘stress’ and subsequent shallow breathing causes a decrease of oxygen to the liver and the resulting decrease of blood flow which ultimately damages the cells of the liver. You’ll learn about more stress relief strategies and the management of stressors in future modules.
And if someone suggests a Milk Thistle supplement then know this .... While St Mary’s thistle (Silybum marianum) has been reported to have hepaprotective properties (protect the liver) conflicting results from different studies make it difficult to determine what effect it has on liver enzymes. And what effect it has on other organs in the body. And the antioxidants that it supplies is available in ANY whole-plant-based food. So, do NOT buy it!!!
I think I have an intolerance to a particular food as I pass a ‘sudden’ bowel movement soon after eating
It is not uncommon for many individuals to link their SUDDEN ‘bowel movement’ to what they JUST ate. But the reasons for a ‘sudden’ bowel movement is multi-factorial.
There are many reasons why you could have a sudden bowel movement... die-off, an infection, eating fast, fear of a particular food, hormone fluctuations, electrolyte balance, an intolerance to the particular ‘quantity’ of a food chemical/component, a virus or food poisoning OR… stress.
But no matter what it is… it will NOT be, cannot be, the food you JUST ate.
The reason is the food you eat will travel this journey…
It will spend 2-3 hrs in the stomach being broken down into a semi-fluid mass (called Chyme).
Then it moves into the small intestine where it starts a journey of travelling the 6-mtrs (20 feet) for another 4-6 hours.
Finally, it arrives in the large intestine where it travels another 1.5mts (5 feet) and 12-15hrs completing the digestive process before you pass a bowel movement.
In total, that’s about a minimum of 18-hrs and a maximum of around 24hrs in a healthy individual.
Therefore, the bowel movement you are passing, is from the food eaten a day earlier (plus other matter e.g. blood cells, dead bacteria etc.). It will NOT be from the meal you just ate, or even the two to three hours earlier!!
The ‘urge’ to pass a bowel movement soon after eating is considered normal, and an important function of the digestive tract to keep things moving. It’s called the gastrocolic reflex (response) and it is responsible for controlling the motility of the gastrointestinal tract. It is most active in the mornings and immediately after meals.
You see… when you eat, the gastrocolic reflex releases a number of hormones to control the movement of food through the intestines. Another function, as the food mass or pressure is increased in the large intestine, is to relax the internal anal sphincter. You then have the urge to pass a bowel movement and your release your external anal sphincter and pass a stool.
If the food in your large intestine has not been thoroughly processed, and peristalsis is too fast, then not enough water is absorbed back over the large intestinal wall and you end up passing a ‘watery’ stool. This can happen when consuming too much oligo-saccharides (sucrose, lactose, maltotriose, etc.) and particularly monosaccharides (glucose, fructose, and galactose) as they are all osmotically active molecules i.e. they draw water into the bowels.
In certain conditions, such as Irritable Bowel Syndrome (IBS), there can be an ‘overreaction’ of the gastrocolic response which comes from the brain-gut axis communication between cortex and the digestive system. This brain-gut overreaction results in diarrhoea or watery stools, and/or accompanying abdominal pain, bloating, diarrhoea, constipation or gas when eating certain foods.
This ‘overreaction’ of the gastrocolic response can also be linked to ‘fear’ or ‘dislike’ of a food. Evidence suggests, that through a number of mechanisms, stress (fear, overwhelm, anger, overthinking, worry etc.) can be a significant factor in the pathophysiology of stress-related faecal urgency, diarrhoea and abdominal distress i.e. increased peristalsis and a sudden bowel movement. You then connect ‘that food’ to your urgent bowel movement, but it isn’t and can’t be. However, you may convince yourself it is THAT food because this pattern actually becomes a self-fulfilling prophecy through the stress/fear/worry response!
The MOST common reason behind ‘gut motility’ (faster - diarrhoea, slower - constipation) is STRESS. Remember this is worry, overthinking, fear etc. not just a big ‘stressor’! Stress has impact on important physiological functions of gut including gut motility, secretion, visceral sensitivity, mucosal blood flow. In addition, stress modifies gut microbiota and enhances paracellular permeability.
Reflect on WHAT was happening, 10-24hrs preceding your ‘sudden’ bowel movement. While different foods process differently in the digestive tract, with some drawing in more ‘water’ to process them the digestive process is largely governed by LIFESTYLE factors such as… Stress, Movement, Hydration, Sleep and HOW you eat i.e. Digestive Dominoes etc.
It is RARELY the food, but it can be a ‘contributing’ factor.
So take your focus away from ‘a certain’ food and instead raise your consciousness and awareness, dig deep, and look into at all the factors that govern your digestion.
POO… what is it and what triggers it to pass?
It’s time for YOU to get (very) comfortable talking about your Poo, Faeces, Stool, Bowel movement, No.2’s....whatever you want to call it.
The reason is, that it tells you so much about your health - especially digestive health. But let's look at some basic information about WHAT IS POO made up of and what triggers its passing… And then… subsequent information about Frequency, Colour, Consistency and Smell will be addressed in other topics.
What is POO (faeces) made up of?
Faeces is about 75% water, undigested food, metabolic waste (ammonia, urea, uric acid, creatinine from protein metabolism) dead cells (from the lining of the gut), dead white blood cells, dead red blood cells, Bilirubin, indigested proteins, fats (incl. Cholesterol), salts, dried constituents of digestive juices, mucous, dead bacteria, some living bacteria and inorganic material such as calcium & iron phosphate … basically an ARRAY of colours mixed together like a palate of paint which determines its colour. And then this COLOUR can change due to the following factors…
What are the trigger(s) to pass a POO (faeces)?
This is the physiological, functional, process of passing a stool…
When we think about or smell food, or food enters the stomach, it triggers the emptying of the stomach’s contents into the first part of the small intestine.
This stimulates mass movements in the large intestine (colon) which moves the faeces towards the rectum (anus). Note… Mass movements are giant contractions that strip an area of its contents.
When the rectum gets distended (gets bigger) this stimulates further contractions moving the faeces towards the anus. Note…The rectum is the final section of the large intestine, terminating at the anus.
This causes a relaxation of the internal muscles known as the ‘Internal anal sphincter’.
Messages are sent to the brain which sends a message to the ‘Defecation reflex centre’. You are then in charge of releasing the ‘External anal sphincter’ and going to the toilet to pass a bowel movement (faeces)
Steps 1-5 are happening all the time as, let’s face it, you are always eating and body is working to eliminate those meals and snacks -- thus it is common to have 3 stools a day.
I have very soft stools, sometimes watery and frequent. What should I do?
The cause of Soft Stools, sometimes watery and frequent, is multi-factorial.
If it's an episode of 'soft watery poos' for a day or too, it can be a result of undigested food moving too fast and thus the large intestine can’t absorb the water fast enough. This can be a result of eating too fast, too much coffee, distracted eating, or stress (worry, overthinking, overwhelm, fear etc).
It can also happen, from time to time during your program, when toxins are being released back into the bloodstream. The body needs to eliminate these 'dangerous' harmful toxins so it speeds up elimination - during this time your stools can be sticky, green, smelly, harder, softer or even covered with mucous. If this is transient, it is nothing to worry about.
After years of eating animal products (meat, dairy, eggs etc), low fibre and packaged or processed foods etc. your gut can react when you start to load it up with an increase in both soluble and insoluble FIBRE from fruits, veggies, nuts, seeds, beans, legumes, grains etc. (i.e. a significant increase in the amount of fibre). Thus it can take a couple of weeks for your Gut Microbiome to settle into its new routine and can result in ‘unusual’ bowel movements that result in multiple ‘toilet’ visits a day (Tip… get some good Gut-Health reading material in the toilet to wile away the time). This is not unusual and nothing to worry about unless it turns into constant diarrhoea, or persists, or is associated with pain. If that’s the case, then a Therapeutic Specific Strain Probiotic may be in order to support your own Gut Microbiome to manage the specific beneficial bacteria involved with IBS-D (Irritable Bowel Syndrome - Diarrhoea)
On your program, you are eating various types of fibre such as…
Soluble fibre… the type of fibre which dissolves in water that forms a gel. This type of fibre helps to lower blood cholesterol and glucose levels. It isn't absorbed in your gut but travels to the large intestines (colon) to feed beneficial bacteria, that then ferment them to produce SCFA’s.
Insoluble fibre… adds bulk to stools, acts like a brush to clean the colon, attracts water into your stool in helping to soften it… supporting regular bowel movements that pass easily.
You are getting BOTH of these types of fibre in equal amounts to balance BOTH the frequency and the consistency of your stools.
One of the reasons for loose stools is that once the food hits the large intestine, the partially undigested parts of the plant-based foods are there for your beneficial bacteria to break down and ferment - essentially eating this fibre. This can take 8-12hrs. However, when the numbers of beneficial bacteria are low, this amount of fibre there can overwhelm their ability to break it down and it is passes quickly through the bowels not giving enough time for water to be reabsorbed across the bowel wall and creating watery poos or diarrhoea. Thus your ‘bowel movements’ are a good indication of the health of your Microbiome thus it is SO important to be tracking this in your PHA.
As your Gut Microbiome improves - numbers, diversity, evenness and function - they will be able to ferment the undigested portion and bowel movements will become more regular.
However, one of the MAIN reasons for soft stools, sometimes watery and frequent, is STRESS… “psychological stress is posited to play either a causal role or exacerbating role in IBS and its symptoms”.
The role of stress, or stressful events, and IBS has been examined extensively and has shown that it is related to the brain-gut axis with…
a) the frequency and intensity of major life events or life changes over the past 6 or 12 months;
b) the frequency and intensity of minor annoyances or hassles over the past month;
c) minor stressful events experienced on a daily or weekly basis for several weeks.
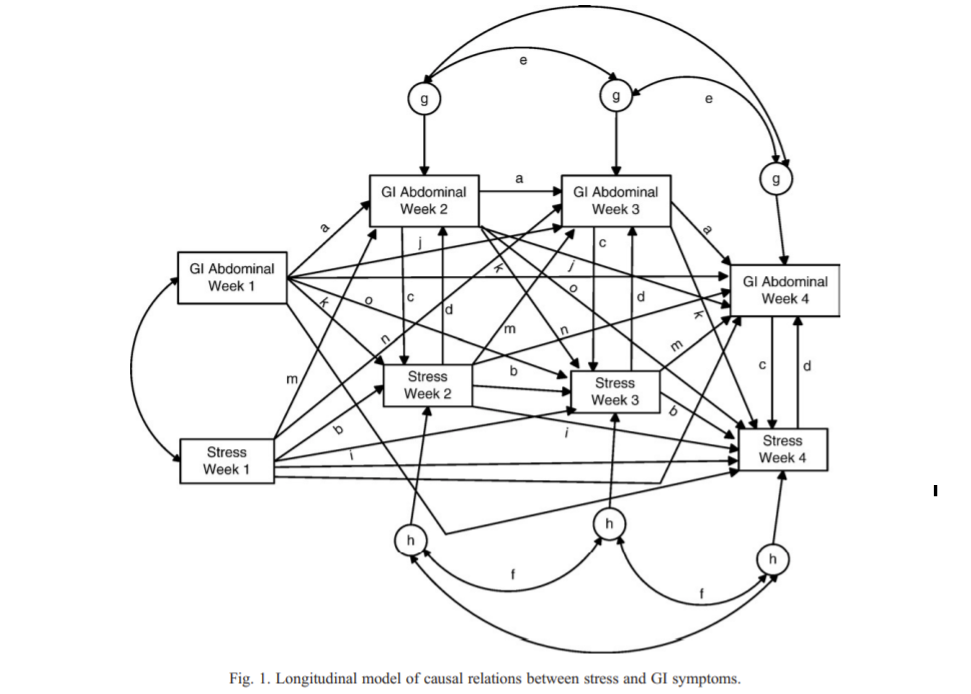
Then on top of this the Gastrointestinal (GI) symptoms experienced as a result of this ‘episode’ (pain, inflammation, intestinal permeability) then creates a new STRESS which then contributes to the cycle continuing. That is… For Week 1 GI symptoms, the causal chain to stress 2 weeks later is the following…
“a) the severity of the symptoms at Week 1 impact the severity of the symptoms at Week 2, which, in turn, impacts the severity of the symptoms at Week 3, which, in turn, impacts stress at Week 3; and |
b) the severity of the GI symptoms at Week 1 has a delayed mediated and independent effect on the severity of symptoms at Week 3, which, in turn, affect stress at Week 3. These dynamics also were evident for Week 4 and the 2 weeks prior to it” see diagram below.
Psychological factors, particularly anxiety and stress… increases colonic paracellular permeability, acceleration of colonic transit and barrier dysfunction through corticotropin-releasing factor (CRF) which leads to episodes of IBS-D, IBS-C and IBS-A (Diarrhoea, Constipation, Alternating) both new and reoccurring.
This also alters the gastrocolic reflex (The gastrocolic reflex is a physiological reflex that controls the motility of the lower gastrointestinal tract following a meal). Individuals with IBS have demonstrated a stronger colonic response to the gastrocolic reflex with experiencing a strong urge to defecate following ingestion of a meal and may experience symptoms like abdominal distension, flatulence, pain, and a persistent and painful desire to evacuate the bowel, despite having an empty colon.
Furthermore, all of these, alter the Gut Microbiome causing a downstream effect that alters the gastrointestinal tract’s ‘paracrine signalling’ (allows cells to communicate with each other) thus indirectly affecting the motility of the colon.
So it is important to do a ‘stress inventory’ of what has been happening in your life. Your stress relief and management modules will teach you techniques to deal with the stress in your life, both at a cognitive level (catastrophic or self-defeating thoughts) and at a behavioural level (problem solving, especially interpersonal problems. Research is clear that a… “reduction in stress, either through a lessening of stressful events or through a reduction in the impact of those events upon the patient, would likely be associated with a reduction in IBS symptoms because of the significant concurrent relations”
What steps to take…
Implement your Barefoot walking, before bed Yin Yoga, Digestive Dominoes and RESONANT BREATHING regularly and consistently.
AND…
Ensure you are drinking water slowly and regularly throughout the day (not all at once)… to rehydrate… Use your Stretch-Decompress-Hydrate method!!
Drink Ginger tea… it has contains ‘gingerol’ an antispasmodic which improves intestinal muscle tone,. Is Anxiolytic which can assist with reducing anxiety. Carminative… can assist in relieving gastrointestinal discomfort when experiencing flatulence and associate symptoms such as bloating.
Reduce or eliminate Caffeine (coffee, tea etc.) Caffeine speeds up peristalsis - the wave-like movement of the muscles that line your gastrointestinal tract which moves food through your digestive system.
Add Gut Health Recipe Compendium recipes of Seeded crispbread/Biome crackers as a side with your breakfast or morning and afternoon snack as this will help to BULK up stools.
If your bottom (anus) area gets sore, or red, then apply a product like these … Organic Baby Balm or Organic Baby Oil … direct to the area. (Apply your GHC10 discount code). Also use a soothing wet wipe, instead of toilet paper, when wiping.
If feeling weak, you may be losing electrolytes. You can make your own simple electrolyte drink by…
o Cut the peel off 1 large lemon, lime or orange and put flesh in blender with 2 cups coconut water, a pinch of pink Himalayan salt, and 2tsp. of raw unprocessed honey. Blitz until liquid. Makes 500ml.
o Sip 200ml (6.7 fl.oz) slowly over a 30 minute period along with your regular water intake. Maximum daily dosage is 1 litre (33 fl.oz). Keep in the fridge in an airtight bottle and shake well before sipping. Keeps for up to 3 days.
o Do not take for more than 3-days. If symptoms persist, or worsen, seek immediate medical advice.
It’s also important to note that there are other reasons for frequent soft watery stools...
A symptom of an infection (gastroenteritis), which can be caused by: a virus – such as norovirus or rotavirus. bacteria – such as campylobacter, Clostridium difficile (C. difficile), Escherichia coli (E. coli), salmonella or shigella; these can all cause food poisoning.
A symptom of gastrointestinal diseases, including Crohn’s disease, Ulcerative and microscopic colitis and celiac disease.
Parasites… testing is required to rule out.
I have very HARD stools. sometimes infrequent, sometimes constipated. What should I do?
Constipation is defined as less than 3 bowel movements a week. Infrequent stools also belong to this category and can include straining, a feeling of incomplete evacuation, or abdominal cramping or pain.
This can be the result of a number of factors...
Metabolic disorders.
Irritable Bowel Syndrome (IBS) or Inflammatory Bowel Disease (IBD).
Neurological conditions such as Multiple Sclerosis (MS), Parkinson’s etc.
Mental health conditions e.g. depression, eating disorders, poor mood etc. As these affect the nerve pathways that control digestive function.
Medications such as opioid pain relievers, antacids, certain antidepressants, antihistamines, some high blood pressure medications and diuretics.
Supplements such as calcium, iron, and high doses of Vitamin D. Calcium and iron, especially, can draw water out of the stool, making it dry and harder to pass.
Protein powders can result in dehydration, and thus constipation.
Structural reasons e.g. bowel obstruction.
Pregnancy hormonal changes (increase in progesterone) can change muscles in the bowel resulting in constipation, as well as an enlarged uterus.
Lifestyle factors – Not enough movement, less than adequate hydration.
Diet... food that has little, or no, water content e.g. processed foods, animal products etc.
Unexpressed emotions e.g. anger, grief, feeling that 'life 'is unjust. Louise Hay, author of ‘You Can Heal Your Life’ talks about the connection between constipation and refusing to release old ideas or being stuck in the past. Her book is a great read with useful tips on how to create new thought patterns - highly recommend!!
Stress... when you are rushed, worried, overthinking, fearful, angry, frustrated etc. it initiates the stress response, which results in a release of hormones which inhibit digestive tract motility and secretions.
The colon has numerous goblet cells scattered along its length and their primary function is to manufacture and secrete mucus. Parasympathetic (rest & digest) stimulation increases the secretory rate of the goblet cells. Sympathetic (fight/flight) stimulation decreases the rate. Less mucous equates a non-lubricated faeces which not only affect the internal lining but exterior area as well, as it is 'dry' and not 'moist'.
The contractions that move faeces towards the anus must be coordinated with the RELAXATION of the internal anal sphincter. As it moves into the rectum, the Parasympathetic reflex which is responsible for most of the defecation reflex
If it is just transient... that is, it happens for a short period of time, here and there during your program... then it may be due to the following reasons...
Stress… not just one major event but a series of 'little' events i.e. overthinking, worry etc. that together cause lots of little mole-hills to become a mountain!
You're dehydrated. With SO much fibre on the your program you have to increase your water intake.
Not enough regular movement. Remember Stretch-Decompress-Hydrate every 30-mins!
Steps to Take to help relieve...
Ensure you are drinking water slowly and regularly throughout the day (not all at once)… Stretch-Decompress-Hydrate!! … to keep things moving.
Add 1 teaspoon of Psyllium Husk in 500ml of warm water, stir really well and drink all at once. This works to 'speed things up' a little. Only do this ONCE a day maximum.
Go for a slow-paced 30-min ‘extra’ barefoot walk... Movement and relaxing helps enormously.
Have a shot of espresso coffee (just one) as it can help to stimulate the bowel (do not do this if you have IBS or IBD). This should NOT be used as a regular 'method' to pass a bowel movement but a 'rare' method if it is getting too uncomfortable.
Massage the lower abdomen in a circular motion after a warm shower/bath.
Drink Ginger tea as it exerts several effects in the gastrointestinal tract GI). It stimulates the flow of saliva, bile and gastric secretions and has been shown to increase gastrointestinal motility without affecting gastric emptying.
Address your STRESS!!!
What does the colour of my poo mean?
The colour of your poo (faeces) is determined, on a daily basis, but what is being excreted by the body and can change on a daily basis depending on what you eat, your body functions, health, stress, infections, dehydration etc.
Faeces is about 75% water, undigested food, metabolic waste (ammonia, urea, uric acid, creatinine from protein metabolism) dead cells (from the lining of the gut), dead white blood cells, dead red blood cells, Bilirubin, indigested proteins, fats (incl. Cholesterol), salts, dried constituents of digestive juices, mucous, dead bacteria, some living bacteria and inorganic material such as calcium & iron phosphate … basically an ARRAY of colours mixed together like a palate of paint which determines its colour. And then this COLOUR can change due to the following factors…
Brown... Light brown to brown is what is considered to be 'in normal acceptable range' however it is important to note that when eating MORE plants (fruit and veggies) or more fats (nuts and seeds) the colour of your faeces can lighten significantly and can even be ‘greenish’ at times.
Pale brown… can occur when ‘fat’s are eaten. Healthy fats in the way of nuts, seeds, avocado etc. Bile (made by the Liver and stored in the Gall bladder) is a greenish-yellow liquid and it aids in the digestion of fats, by breaking them down into fatty acids. The mix of greenish-yellow + brown + veggies = a pale brown stool.
Yellow... If faeces moves through the intestines too quickly, or when you consume more fats, it can be more of a ‘tan’ ‘yellowish’ colour. However, it is important to note that infections can result in yellowish faeces so you should keep an eye on it.
Dark Brown Black... Eating foods such as black licorice or blueberries can darken faeces. Animal products such as beef, lamb etc. can give faeces a darker hue.
Black... Generally from iron supplements. Or if faeces spends too long in the bowel. A sign of inflammation.
Red... Danger 🆘 Seek immediate medical assistance ASAP. Can be from haemorrhoids but should be checked. Having said that, if you’ve eaten beetroot, it can cause faeces to be blackish red, or even pink, and can freak you out!
Green... Increased vegetable consumption. This is VERY common in the earlier phases where an increase in green veggies can make faeces a greenish colour. Excess sugar consumption can also make faeces green.
Grey... When there isn’t enough bile produced. Bile is what is released by the gallbladder (liver) to break down fats. You should keep an eye on this.
White… White or a very pale grey stool could be indicating that there is a biliary obstruction. That means the bile duct is blocked. If the Bile is not entering the GI tract then the ‘bile pigment’ is not getting mixed with the stool.
Blue or strange colour… can happen with certain medications — but the change is usually as long as the medication is taken.
So, as you can see there is a lot of factors that can influence the colour of your faeces. If you're concerned, please post in the LIVE Q&A Broadcast post, or book a consult if you prefer. And if you are worried, book an appointment with your GP.
My Poo smells bad, is that normal?
For faeces to ‘smell’ slightly unpleasant is considered to be a ‘normal acceptable range’. But if faeces have a strong putrid and foul smell, that is ongoing, then DO NOT ignore, further investigation by a specialist is required. But a not so aromatic 😊 bad smell intermittently… is multi-causative and isn’t usually a cause for concern. Here are some of the causes…
An increase in Fats… From nuts, seeds, coconut etc. which can putrefy and smell, from time to time, if the body isn’t digesting the fats well. This can be from eating too fast. Remember digestion starts in the mouth with salivary lipase breaking down fats!! Other reasons are that your body may not produce enough lipase (fat-digesting enzyme) or bile salts. If that's the case these ‘fats’ are not broken down and may result in increased fat excretion and foul-smelling stools. This is an issue if the Gall Bladder has been removed. If this is accompanied by a ongoing oily bulky or floating stools and leakage, then further medical investigation is required. Fat in the stool is greater when whole nuts, on their own, are eaten, as opposed to nut milks or meals with nuts in them, as they are less well absorbed.
Medications... Detoxified by the liver and then excreted by the bowels may cause bad smelling stools. You may not have smelt them before due to the pungency of previous eating of processed foods or animal products. With those out of the picture, you may be smelling this. Some medications block the enzymes that digest fat which can result in smelly oily stools.
Slow transit time... If you don't go to the toilet regularly for a bowel movement, then the food you have eaten is lingering in a warm (37°C/98°F), moist environment in the colon resulting in it smelling more.
Infections... Can result in foul-smelling stools. This can happen from contracting a virus, parasites or from eating contaminated food with E. coli or Salmonella. Often accompanied by other symptoms such as diarrhoea, fever, pain etc.
Die off… Also known as the Herxheimer reaction (Jarisch-Herxheimer reaction). Toxins from dying pathogens (viruses, bacteria, parasites, candida, etc.) overwhelm the body’s abilities to clear them out. Not only causing symptoms but also affecting bowel movements. Faeces can intermittently smell bad, really bad. But this should improve as you move through your program.
An Increase in Insoluble fibre… With foods such as oats, lentils, psyllium husk, fruits and vegetables can result in a short period of ‘foul-smelling’ stools. The reason is that the insoluble fibre acts as a scrubbing brush ‘scouring’ the intestinal tract. It's a good thing though as it further generates the production of mucous that protects the colon wall and helps to move through foods – sort of like a lubricant.
Types of fibre… Can increase faecal mass. For example, degradable fibres such as cabbage and apple can increase the number of bacteria excreted – more bacteria excreted more smell. “The effect a particular fibre has on colonic function therefore depends on its digestibility and thus its physical and chemical composition”. [1] Meaning that the ‘smell’ can change depending on what type of fibre you have eaten. Some vegetables contain more sulphur which can make stools smell more pungent almost like a ‘rotten egg’. Cruciferous vegetables are high in sulphur (bok choy, broccoli, cabbage, cauliflower, kale, kohlrabi, radish, watercress etc.) Also, garlic, onion, legumes.
Characteristics of your UNIQUE Microbiome… Can result in having a completely different smell than someone else eating the exact same food. “The differing response of individuals to the same fibre source may relate to the characteristics of their colonic bacteria”.
Malabsorption of food… Can cause food to be undigested and in the warm and moist environment of your colon can produce gases and a change to the colour, frequency and smell of stools. There are a number of reasons for malabsorption from simple reasons as eating too fast (not following Digestive Dominoes) or Food intolerances to starches, sugars, diary proteins or fats. Or the result of more serious conditions such as Coeliac disease, Bacterial overgrowth, Inflammatory bowel disease (IBD), Irritable Bowel Syndrome (IBS), Pancreatitis etc.
Antibiotic treatment… Can result in foul-smelling stools as it disrupts beneficial bacteria colonies. Generally, this is restored after high-dose multi-strain therapeutic Probiotics, Saccharomyces boulardii (SB) a biotherapeutic probiotic agent and also feeding with a variety of fibre types to re-establish diversity, numbers and function.
Serious medical conditions… Can cause foul-smelling stools so if it is ongoing and accompanied by fever, blood in stool, black stools, pale yellow stools, nausea, constipation or diarrhoea, pain in the chest or around the heart or even in the back between the shoulder blades or difficulty in swallowing immediate medical investigation is required.
Supplements can increase sulphur levels…. Including but not limited to Omega 3’s, Garlic capsules, Magnesium supplements, N-acetyl cysteine (NAC).
Lots to digest I know (excuse the pun) but the message is that the ‘odour’ of your stools is multi-causative and if you’re getting an occasional stinky stool, don’t be worried. Your diet is changing dramatically, with a huge increase in fibre and this can have a short-term impact on stool ‘odour’ ‘frequency’ and ‘consistency’.
It is though, an important lesson - ALWAYS look at your faeces as they tell you SO much about your health.
So… what IS a normal Poo?
While there is a range of what is considered to be in a 'normal acceptable healthy range' there is NO normal poo (faeces).
Why?
Because the excretion of faeces is based on a number of factors, that change daily…
WHAT you have been eating and drinking (fibre, carbohydrates, protein, fats etc.)
Amount of body and blood cells excreted that day.
Some mucous (from normal gastrointestinal lining) … more if you have inflammation.
Dead and some living bacteria.
And of course… HOW you eat, hydration levels, movement, sleep and stress levels.
So many factors affect the consistency, colour, frequency and smell of faeces. Therefore, you may go through times of firmer faeces, then softer, then not formed, then fully formed, then greenish, then small pieces, then sinking, then floating, then one long fully formed piece, then sticky, then.... you get the picture right.
The takeaway is that it changes daily… thus there is NO normal. Having said that there are two extreme's that are NOT considered to be in a normal acceptable range and should be further investigated by a specialist…
Constant daily watery diarrhoea-like stools (and constant urgency ).
Constant hard small pellet, hard to pass stools (and constant straining).
But having 'faeces' that change daily is considered to be normal and nothing to worry about.
I have Sticky Poos Is This Normal?
Ever noticed that your poo (faeces) sometimes sticks to the side of the toilet bowl? And appears greasy and sticky?
Well there are a few reasons this can happen…
Too much fat in the diet - excess fat beyond what can be absorbed ends up in your stool, making greasy and sticky.
Gluten intolerance (due to ‘too’ much) where you can’t properly digest the protein ‘gluten’.
Lactose intolerance.
And if going on for prolonged periods, and accompanied by abdominal cramps, bleeding or excessive gas, it can be a sign of inflammatory digestive disorders such as Crohn’s disease or Ulcerative Colitis.
The good news is that, if not chronic, it is easily fixed…
Drink water regularly and slowly water.
Reduce the amount of saturated fats you are consuming ESPECIALLY animal (saturated) fats.
I have quite a bit of flatulence and sometimes it really smells. Is this normal?
No matter what you call it… Flatulence, Fart, Frog, Bum Burp, Gas, Break Wind, Ass Acoustics… it is a bodily function that we ALL do. But sometimes it can be over the top, painful or just downright embarrassing. But for the most part, passing ‘gas’ is 'normal' with most people passing gas multiple times a day - you just don't know about it as it's not a common subject of discussion ;-)
Flatulence, whether 'smelly' or just 'gas' on its own is nothing to worry about, but if it’s accompanied by other frequent symptoms such as pain, spasms, unusual bowel movements, nausea, weight loss, blood in stools etc. then further medical investigation is required.
Also excessive or constant putrid gas can be a sign that that your Gut Microbiome is out of balance - dysbiosis. It can resolve itself during your program as you restore the function and diversity of the Gut Microbiome. However, as it can be related to more serious conditions such as Inflammatory Bowel Disease (IBD) do not put off further medical investigation if it doesn't resolve.
There are reasons why from time to time you may have extra smelly gas, or more frequent. These are…
You’ve eaten too fast and your digestive tract can’t break these foods down, so they hang around in your gut for longer and ferment, which can result in gas, sometimes smelly.
You’ve been talking while eating and swallowed too much air.
You’re drinking carbonated beverages such as Soda or Sparkling Mineral water.
Drinking red wine. It contains naturally occurring sulphites (and sometimes some added). This can result in rotten-egg smelling gas.
Eating processed foods with added sulphites. This can result in rotten-egg smelling gas.
Cruciferous veggies, garlic and onion are rich in sulphur which can cause a rotten-egg smell type of gas. Sometimes the combination of these in meals over a couple of days can result in putrid gas, but it will pass.
On your program increasing your fibre intake significantly. At times this can overwhelm your gut bacteria’s ability to break it down and can result in gas building up in the colon. Most foods won’t cause an odour however, others result in the formation of sulphur-containing gases which can sometimes smell like a rotten egg.
Your Microbiome is unique to you and you may possess certain types of gut flora that produce more gas or smellier gas.
Beans, Legumes and Cruciferous veggies contain galacto-oligosaccharides (GOS). The gastro-intestinal tract lacks the enzyme needed to break down these sugars so relies on gut bacteria to do the job. If you lack the function and diversity in beneficial bacteria it will overwhelm its ability to break it down. Try cutting down the portion of these by a third and test again. Over time you will get better at digesting. Also eat canned and rinsed legumes as they have lower levels of GOS than the dry, soaked and rinsed legumes.
Cysteine is a protein (amino acid) that is sulphur-containing. It is essential for metabolism and detoxification however foods containing this protein can result in stinky hydrogen sulphide emissions.
Some fruits aren’t always absorbed well by some, especially those higher in fructose like grapes or watermelon. Therefore, you may end up extra gassy whenever you eat them.
Some medications are poorly metabolized and can cause excess gas.
You have an infection.
You have a food intolerance. But you would soon know this as it would happen over and over again with the same food. If you suspect this, then keep a food diary to track symptoms.
But whatever type of gas, know that it is fine to hold it in for a SHORT amount of time (let’s say you have a meeting) but if you hold it in for a long time you’ll end up bloated and feeling very uncomfortable.
Lemon Ginger - Digestion, Hydration and more
Starting your day with a refreshing large warm mug of warm water (275-375ml) with a Lemon-Ginger blend cube, followed by another glass of water (250ml) hydrates the body after hours of sleeping.
Lemon juice on its own has benefits for your health; but the REAL BENEFITS come when including the peel, seeds AND pith (the white bit) as it is packed with Vitamin C, Calcium, Potassium, Bioflavonoids, powerful Antioxidants AND Pectin a powerful prebiotic that promotes the growth of beneficial bacteria. The pith and peel help to enhance Vitamin C absorption, and contain Hesperidin, which may assist with capillary function helping to relieve leg cramps. It is also high in Rutin and Quercetin, antioxidants that have powerful anti-inflammatory benefits. Quercetin is a great antihistamine; proven to reduce allergies.
Add to the mix GINGER which has been repeatedly confirmed, through scientific studies, to being highly effective for pain relief and reducing inflammation, amongst its other powerful therapeutic and preventive effects such as its… anti-allergic, anti-viral, antispasmodic, antibacterial, antiemetic, antihistamine, anti-inflammatory, anti-nematode, antioxidant, antiseptic, anxiolytic, carminative and diaphoretic properties. In addition, it exerts beneficial gastrointestinal activity by stimulating the flow of saliva, bile and gastric secretions which increases gastrointestinal motility without affecting gastric emptying. It can assist with relieving indigestion, poor appetite and spasms of the digestive tract and…
“Ginger exerts potential protective effects on the gastrointestinal membrane and lowers the chances of mucosal injury”.
“It has been reported that dietary ginger altered the permeability and fluidity of the intestinal membrane, resulting in increased absorptive surface of the small intestine with an increase in microvilli length”.
“Ginger also increased the absorption of zinc, iron, β-carotene and calcium in the intestines.”
“Ginger relieved pain and swelling to varying degrees in patients with osteoarthritis, rheumatoid arthritis, and muscular pain without causing serious adverse effects even after long periods of use.”
It is a great alternative to waking up with tea or coffee (caffeine)
Although Lemon is known as an acidic fruit; when broken down in the body, its minerals are detached in the bloodstream creating an alkalizing effect on the body. Also, because 1 lemon contains around 4-drops of lemon oil, you are also getting oil mixed in.
However, it is important to think about ‘teeth’ health as well so it’s important that you…
Mix your Lemon-Ginger cube in a large glass of water, not a small glass.
You have the option to drink your Lemon-Ginger through a straw, to bypass teeth.
Always follow with a glass of water, this rinses the mouth, removing any acid that may remain on the tooth surface.
Eat after your Lemon Ginger (i.e. breakfast) as this produces more saliva, neutralising the acidity in your mouth.
Do not brush your teeth for at least 30 minutes after drinking your Lemon Ginger. This goes for tea/coffee too! Do NOT brush your teeth within 30-mins of a coffee or tea as the acidity softens tooth enamel and the brushing affects the teeth.
Don’t ‘scrub’ teeth aggressively as this causes ‘mechanical’ wear and tear on tooth enamel.
REFERENCES: Every endeavour has been made to find a reliable base of evidence (peer reviewed studies, studies, reviews, meta-analysis, articles) and ensure they are free from commercial interests.
Chronic psychological stress in rats induces intestinal sensitization to luminal antigens. Am J Pathol. 2006.
Effects of chewing on appetite, food intake and gut hormones: A systematic review and meta-analysis. 2015.
The effects of psychological stress on the esophagogastric junction pressure and swallow-induced relaxation. Gastroenterology 1994.
Proton pump inhibitors affect the gut microbiome. Gut 2016.
Gut microbiome, liver immunology, and liver diseases. 2021.
The role of the gut microbiome in chronic liver disease: the clinical evidence revised. 2019.
The role of dietary fibre in the human colon. Canadian Medical Association journal. 1980.
Motivational Non-directive Resonance Breathing as a Treatment for Chronic Widespread Pain. 2019.
Positive effect of abdominal breathing exercise on gastroesophageal reflux disease: a randomized, controlled study. 2011.
The effects of slow breathing on affective responses to pain stimuli: an experimental study. 2010.
The effect of transcutaneous vagus nerve stimulation on pain perception–an experimental study. 2013.
Direct evidence for spinal cord involvement in placebo analgesia. 2009.
A friendly reminder…
♥ Need a little extra support or a deep dive into your personal health issues? As an optional add-on, you can book one-on-one consults at the 50% off member rate. Sessions are offered in person, or via FaceTime, WhatsApp, or Zoom video. Perfect if you’d like personalised advice or tailored coaching alongside the group program. The Private Consult link is in your Member Hub.
♥ This is a group online coaching program, therefore any direct questions, comments or messages to Practitioners, received through the Gut Health Circle, Email, Text, Messenger, Social Media etc. are not looked at, nor replied to. Please join the ZOOM roundtables or book a consult to connect with Pracitioners.
♥ For any administrative inquiries, such as accessing your account, please contact the Customer Support team directly at hello@nataliewoodman.com. Please note, administrative questions do not relate to program-related support or how to navigate the program.
♥ A lot of time has been spent in developing and perfecting this program for YOU. Please respect our work, and how our team makes its’ living and do NOT share, copy, reproduce, redistribute, screenshot ANY part of the program to anyone through any medium. The entire program is subject to copyright.
♥ Please re-read our Terms and Conditions if unsure of your rights and responsibilities.